Gastroparesis is a condition that affects the stomach nerves and muscles, causing the movement of food from one’s stomach to their small intestine to slow or stop.
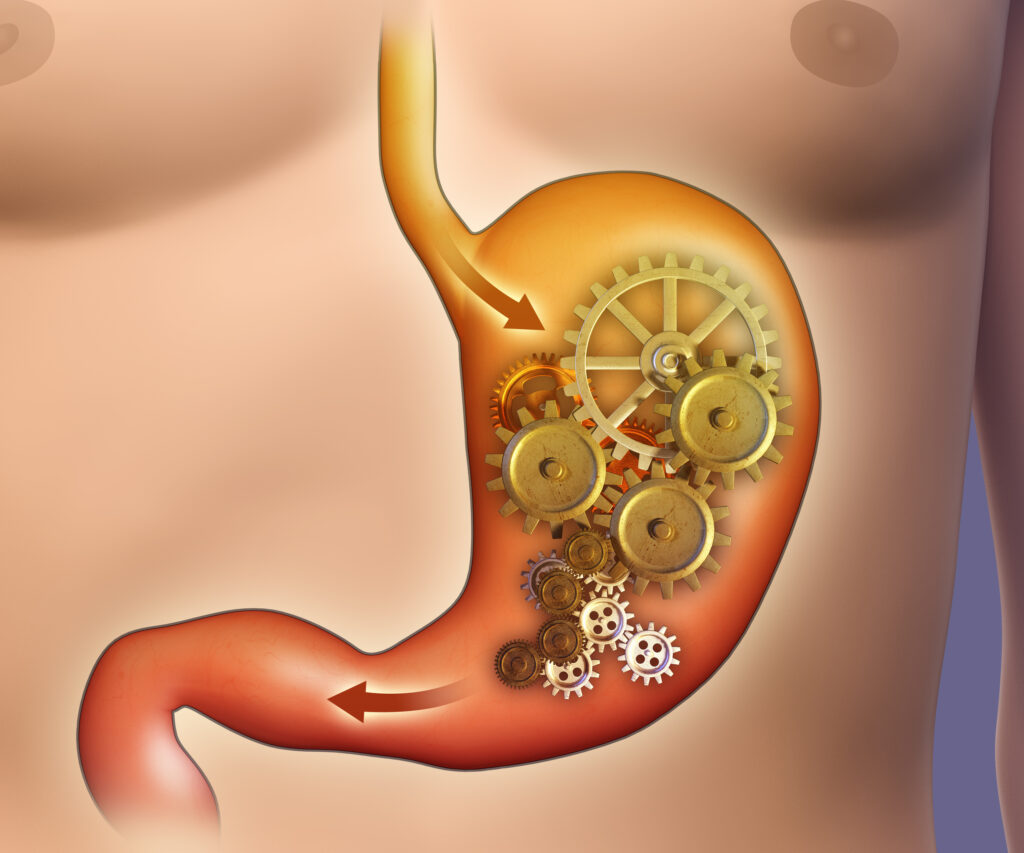
Under normal circumstances, the stomach relaxes after ingesting food, which prevents a sense of fullness and allows the stomach to adequately digest the food. The stomach muscles then push, grind, and mix the food until emptying the solids into the small intestine. For those with gastroparesis, one or more steps in that process don’t function like they should and food stays in the stomach instead of moving through the rest of the digestive process. There are several tests that can help diagnose this condition.
Common symptoms of gastroparesis are:
- Feeling full shortly after starting a meal
- Nausea
- Bloating
- Vomiting
- Acid Reflux
- Changes in Blood Sugar levels
- Abdominal Pain
Long term, gastroparesis can lead to:
- Weight Loss
- Dehydration
- Malnutrition
Some people with gastroparesis will have very little signs or symptoms. It is also important to understand that the symptoms above can have a variety of other causes involving the digestive system — or a different part of the body altogether.
Who is affected by this condition?
Up to half of those who develop gastroparesis have no underlying cause. While it can happen to anyone, having a diagnosis of certain other conditions can increase one’s risk. Examples include those with long-standing diabetes, certain neurologic or rheumatologic conditions and those on certain medications. Additionally, those with damage to the vagus nerve can trigger problems with motility that leads to gastroparesis.
How is gastroparesis treated?
Gastroparesis is chronic, meaning it cannot typically be cured. However, there are options that can offer some relief.
Common recommendations include getting the underlying health condition under control or reducing/stopping the medicine believed to be the cause. To help relieve symptoms, medications that reduce nausea and vomiting may be prescribed as needed.
Following dietary guidelines can help most patients experience some form of relief. Specific diets are available, but in general it is recommended to:
- consume smaller, more frequent meals.
- stay well-hydrated.
- limit fat and insoluble fiber.
- chew food completely before swallowing.
- eat soft, well-cooked foods.
- avoid carbonated beverages.
- avoid alcohol.
- get some gentle physical activity after a meal, such as taking a walk.
- avoid lying down for 2 hours after a meal.
- take a daily multivitamin.
Some patients may find the most benefit by shifting to a full-liquid diet that includes supplemental nutritional drinks. This can be particularly helpful when symptoms flare up.
Is surgery an option?
Endoscopic and surgical options may be recommended for those who have tried other avenues and do not experience relief. However, a thorough evaluation by a medical professional is essential before this would be considered.
Final thoughts…
Gastroparesis itself isn’t typically life-threatening, however — it can certainly be life-altering, and its long-term symptoms can lead to serious complications. It is important to properly manage the condition, so that risk becomes very minimal. As each patient’s experience with the condition is unique, an ongoing and individualized treatment plan under the care of a specialist is recommended.